
SPRINGFIELD – Career and technical education teachers will now be granted tenure under a new law sponsored by State Senator Meg Loughran Cappel.
“I’ve been a strong advocate for CTE, which gives students the opportunity to receive a hands-on academic experience,” said Loughran Cappel (D-Shorewood). “With the ongoing teacher shortage, we need to ensure CTE teachers receive the benefits they are entitled to and deserve.”
Senate Bill 463 allows CTE teachers to be granted tenure if they have a license with credentials. Loughran Cappel’s law aims to expand tenure eligibility from only educators with a Professional Educator License to include CTE teachers.

SPRINGFIELD – Funding for special education students will be more equitable under a new law sponsored by State Senator Meg Loughran Cappel that creates a fair reimbursement rate for special education day schools.
“Since joining the General Assembly, I have worked to ensure all special education students receive a quality education in the least restrictive environment,” said Loughran Cappel (D-Shorewood). “With this law, all special education day schools will see equitable funding opportunities, no matter the student’s placement.”
Senate Bill 3606 equalizes the reimbursement rate received by public school districts from the Illinois State Board of Education when sending high-needs special education students to private and public special education day schools.
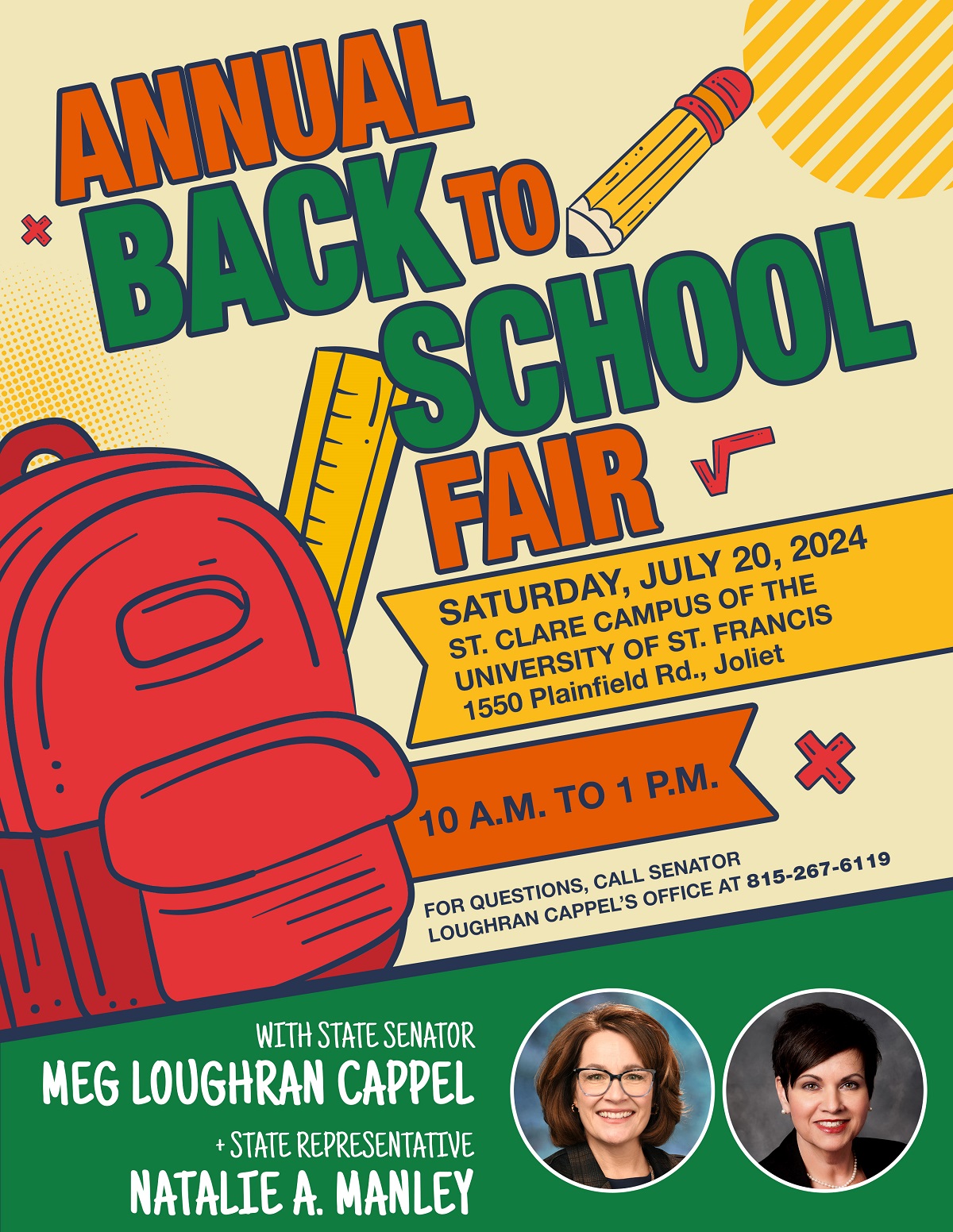
JOLIET – Families can get their kids ready to head back to the classroom by attending State Senator Meg Loughran Cappel and State Representative Natalie Manley’s Back to School Fair on July 20.
“The school year will be here before we know it,” said Loughran Cappel (D-Shorewood). “It’s a perfect time to have an event that serves as a central location for connecting families with programs in our community. We want families to have a chance to get free school supplies and useful resources all in one place.”
The free event will take place from 10 a.m. to 1 p.m. on Saturday, July 20 at the University of St. Francis St. Clare Campus, located at 1550 Plainfield Road in Joliet. Loughran Cappel and Manley will be joined by community partners who will provide resources and supplies for students to use when they return to the classroom. Students can receive free school supplies at the fair and learn about a number of services offered by organizations in the community.

SPRINGFIELD – To streamline the administration of early childhood education programs and services, State Senator Meg Loughran Cappel supported a new law creating the Illinois Department of Early Childhood.
“Illinois has been a champion in education, ensuring every child is set up to be a lifelong learner at an early age,” said Loughran Cappel (D-Shorewood). “As a former educator, I’m confident this is a necessary step for kids across the state to be given more opportunities to succeed with the support, resources and stability they need and deserve.”
Senate Bill 1 creates the Department of Early Childhood to be the lead agency for administering and providing early childhood education and care programs and services to children and families in Illinois. The new agency will be dedicated to making access to such state programs easier for parents and providers to navigate.
Page 13 of 73